(Focus keyword: depression and sleep loss)
Introduction
Many people struggling with mental health find that depression and sleep loss go hand in hand. You may notice trouble falling asleep, waking up often, nonrestorative sleep, or even oversleeping. This blog dives into why depression causes sleep problems (insomnia or poor sleep), what signs to watch for, and practical ways to improve sleep when depressed. Use this as a guide (not medical advice) and consider professional help if symptoms persist.
(That video gives a good visual explanation of how poor sleep affects mental health and brain functions.)
Also, here’s a video directly about depression + sleep disturbance:
Depression and Sleep by Psych Hub YouTube
1. Understanding the Link: Why Does Depression Cause Sleep Loss?
1.1 The two-way relationship
- Depression often disrupts sleep architecture (how you cycle through stages of sleep).
- Sleep disturbances can worsen mood, create emotional dysregulation, and increase depression symptoms.
- Sometimes it’s hard to tell: did insomnia lead to depression, or did depression cause insomnia? (See “depression vs insomnia which comes first”.)
1.2 Biological & psychological mechanisms
| Mechanism | What Happens | Effect / Relevance to Depression & Insomnia |
|---|---|---|
| Neurotransmitter dysregulation | Serotonin, norepinephrine, GABA are imbalanced | Makes it harder to fall asleep or maintain sleep |
| HPA axis / stress hormones | Elevated cortisol, overactive “fight-or-flight” tone | Nighttime arousal, racing thoughts |
| Inflammation & cytokines | Elevated inflammatory markers | Linked to both depression and poor sleep |
| Circadian rhythm disruption | Internal clock (melatonin, light cues) is misaligned | Difficulty initiating or maintaining sleep |
| Cognitive / emotional rumination | Worrying, guilt, self-criticism, negative thoughts | Keeps mind active instead of restful |
| Comorbid anxiety | Many depressed individuals also have anxiety | Anxiety magnifies sleep disturbances |
These are some of the causes of sleep loss in depression and factors linking depression and sleep disturbance.
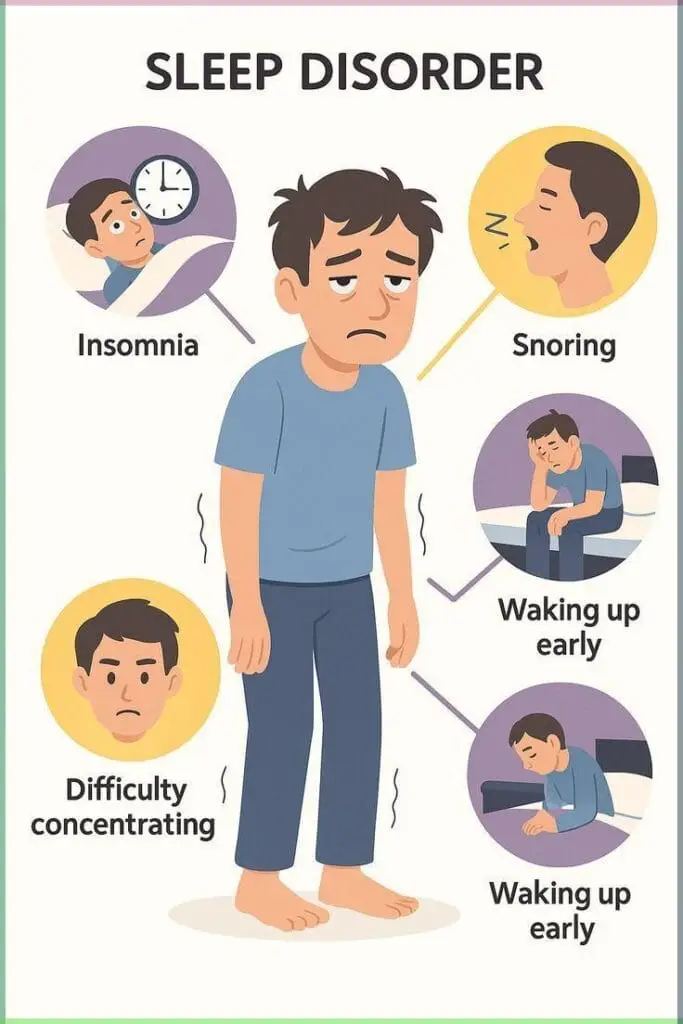
1.3 Types of sleep problems common with depression
- Difficulty falling asleep (sleep onset insomnia)
- Frequent awakenings / fragmented sleep
- Early morning waking (waking too early)
- Nonrestorative sleep (you sleep, but feel unrefreshed)
- Hypersomnia / oversleeping (in some depression types)
These fall under “sleep problems in depression” or “depression and sleep disturbance.”
2. Q&A: Common Questions
Q: Is insomnia a sign of depression?
A: Yes, insomnia comorbid with depression is very common. Many people with depression report sleep loss, poor sleep, or waking early. Disturbed sleep may appear before mood symptoms in some cases.
Q: How do I know if my sleep issue is due to depression or something else?
A: Look for symptoms of depression and insomnia together (persistent low mood, loss of interest, fatigue). If sleep issues are accompanied by mood change, changes in appetite, concentration, it’s more likely to be depression-related.
Q: u003cemu003eCan fixing sleep resolve depression?u003c/emu003eu003cbru003e
A: Improving sleep helps, but usually doesn’t replace therapy/medication. Treating depression and insomnia together (e.g. CBT for insomnia plus antidepressants) often yields best results.
Q: Why do I wake up early when I’m depressed?
A: Depression can shorten the “sleep maintenance” period — the brain may push you awake early. Also, hyperarousal (stress hormones) may trigger early awakening.
Q: Are there natural remedies / lifestyle changes that help?
A: Yes — sleep hygiene, relaxation techniques, mindfulness, diet, light exposure, structured routines can aid. These fall under how to improve sleep when depressed or sleep hygiene for depression.
3. Signs & Symptoms: How Sleep Loss Manifests in Depression
Below is a table summarizing common indicators of sleep disturbance in depression:
| Sign / Symptom | Description | What It Suggests |
|---|---|---|
| Difficulty falling asleep | Lying awake for long periods | Sleep onset insomnia |
| Frequent waking | Waking multiple times at night | Sleep fragmentation |
| Waking too early | e.g., waking at 4–5 am and unable to go back to sleep | Early morning wakening |
| Daytime fatigue | Feeling exhausted despite “sleeping” | Nonrestorative sleep |
| Mood worsening in morning | Mood is worse in early hours | Depression-related sleep pattern |
| Oversleeping / sleeping too much | Sleeping > 9 hours | Hypersomnia (less common subtype) |
| Cognitive fog, trouble concentrating | Brain feels “slow” | Sleep loss → impaired cognitive function |
These are “signs of sleep problems in depression” / “symptoms of depression and insomnia.”
Example: A 25-year-old student may say, “I fall asleep late, wake at 3 AM, can’t go back to sleep, then drag through classes with brain fog.” That’s a real scenario echoing depression and insomnia.
4. How to Fix It: Strategies, Treatments & Lifestyle Changes
Here’s where we move from why depression causes sleep issues to how to treat / improve sleep loss due to depression. Use these under “how to fix depression-related insomnia” / “sleep hygiene for depression” / “how to treat sleep loss due to depression”.
4.1 Sleep hygiene & lifestyle tweaks
- Maintain a consistent sleep schedule (same sleep & wake times)
- Create a restful environment (dark, quiet, cool room)
- Limit screens / blue light exposure 1 hour before bed
- Avoid caffeine / stimulants in late afternoon/evening
- Moderate alcohol / nicotine use (they fragment sleep)
- Get daytime light exposure (morning sunlight helps circadian rhythm)
- Exercise regularly, but avoid vigorous activity close to bedtime
- Healthy diet (avoid heavy meals late)
These are part of improving sleep habits for better mood.
4.2 Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT for insomnia is a structured therapy that addresses thoughts and behaviors maintaining insomnia. In depressed individuals, combining CBT-I with depression therapy is effective.
Components include: sleep restriction, stimulus control, cognitive reframing, relaxation training.
4.3 Relaxation & mindfulness techniques
- Deep breathing (4-7-8 method)
- Progressive muscle relaxation
- Guided imagery / visualization
- Mindfulness meditation / body scan
- Yoga nidra
These help calm rumination / anxious thoughts at night.
4.4 Chronotherapy & light therapy
- Bright light therapy (in morning) helps reset circadian rhythm
- Delayed sleep phase or advanced phase adjustments
- Exposure to natural light outdoors
4.5 Medical & professional approaches
- Talk therapy (CBT, interpersonal therapy) — treat depression and insomnia together
- Antidepressants (some can help sleep; some disturb it)
- Sedative / hypnotic medications (short-term)
- In severe cases, wake therapy (sleep deprivation therapy) has been used under medical supervision in mood disorders Wikipedia
4.6 Supplements & herbal options (with caution)
- Melatonin
- Valerian, chamomile, lavender (evidence is mixed)
- Always consult a professional before trying these
5. Step-by-Step Plan: What You Can Try This Week
Here’s a 7-day plan (as an example) to begin improving sleep despite depression:
| Day | Focus | Action |
|---|---|---|
| Day 1 | Track & assess | Keep a sleep + mood diary (time to bed, wake, awakenings, mood) |
| Day 2 | Sleep hygiene set-up | Adjust environment (blackout curtains, noise control) |
| Day 3 | Fixed schedule | Decide your “sleep window” and stick to it (e.g. 10 pm–6 am) |
| Day 4 | Light exposure | Get 15–30 min morning sunlight; dim lights in evening |
| Day 5 | Relaxation practice | Do 10–15 min guided meditation before bed |
| Day 6 | Wind-down routine | No screens, gentle stretch, journaling, reading |
| Day 7 | Review & adapt | Check diary, see what’s working; tweak as needed |
Over time, gradually incorporate CBT techniques, therapy, and/or medical support.
6. Common Mistakes & Pitfalls
- Trying to “catch up” sleep by oversleeping (backs bounce back)
- Napping excessively during day
- Using screens / phones late — blue light suppresses melatonin
- Alcohol or heavy meals before bed
- Ignoring mood symptoms (just treating sleep)
- Expecting overnight miracles — improving sleep often takes weeks
7. Internal / External Links
Internal Links (you can adjust to your existing blog)
- “10 Self-Care Routines for Better Mental Health” — link to self-care post
- “Signs of Depression: When to Seek Help” — link to your article on depression symptoms
- Mindfulness Exercises You Can Do in 5 Minutes”
External Links
- National Institute of Mental Health (NIMH) – Sleep and Sleep Disorders (for general medical reference)
- American Academy of Sleep Medicine
- CBT for Insomnia (CBT-I) clinical resources
- Link to research such as wake therapy on Wikipedia Wikipedia
8. Example Narratives / Case Illustrations
Case 1: Student struggling with exam stress & depression
Ravi, a 20-year-old college student, began feeling persistent sadness and low motivation. He started going to bed around 2 am, but his mind kept racing. He woke at 4 am, unable to go back to sleep, then struggled all day. He thought it was exam anxiety, but soon noticed mood worsening. By adopting a fixed sleep window, doing 10 minutes of guided meditation each night, and talking to a counselor, he saw gradual improvement in both mood and sleep.
Case 2: Working professional with evening overthinking
Priya worked through remote meetings till 9 pm, then would scroll social media until late, thinking over work issues. She found herself unable to wind down, waking at 3 am. She introduced a “digital curfew” (no screens after 9 pm), dim lights, and a bedtime journal. Over weeks, her awakenings reduced, and mood stabilized.
Such examples resonate with depression causing sleep loss, sleep disturbances and mood disorders, and improving sleep in depression.
9. When to Seek Professional Help
If you experience any of the following, please reach out to a mental health professional:
- Persistent insomnia or hypersomnia lasting ≥ 2–3 weeks
- Worsening depression symptoms (suicidal thoughts, extreme hopelessness)
- Major impairment in daily functioning
- No improvement despite trying strategies
Professionals may offer therapy, medications, or combined treatment plans.
10. Conclusion
Depression and sleep loss form a vicious, bidirectional cycle: depression disrupts sleep, and poor sleep worsens mood. But it’s not hopeless. With sleep hygiene, therapeutic techniques (like CBT-I, relaxation, chronotherapy), and professional support, many people see meaningful improvement.
This blog help me lot in my life